QEII Halifax Infirmary Emergency Department is working with reduced space, which may lead to delays for those with less urgent concerns. Learn more here.
Starting Saturday, December 14, the entrance to the QEII Halifax Infirmary Emergency Department will change to 1840 Bell Road. Learn more.
Nursing provides unique career path
Dr. Susan Johnson claims she has the “coolest job at Nova Scotia Health.” She’s the manager of the Technology Enabled Practice team, a group of seven people who support clinical teams in bringing new technology, or other solutions, to the workplace.
“We look at clinical issues, things that clinicians identify as barriers to providing the best care that they can, and we come up with solutions.”
The team came together in early 2021 when it became evident there was a gap in this kind of clinical support. Since then, her team has worked on innovative projects like the automated medicine dispensing cabinet implementation, the Smart Bed pilot, and research into home IV infusion.
“In a big organization it’s challenging to make a significant difference that has impact across the province. When I'm talking about difference, it's making efficiencies for staff, improving patient outcomes, and reducing safety incidents. It has impact and it's meaningful.”
Not all solutions are technical
Not all the problems her team works on are solved by technology. The team launched a project where they travelled around the province to see how IV fluids were being stored at regional facilities.
They identified a range of recommendations to improve process, like clearer labeling, color coded bins, and better storage organization. Johnson says there are a lot of simple fixes they can recommend after looking at the bigger picture.
“Once finalized, the Institute for Safe Medication Practices Canada is looking at using our research to publish Canada-wide recommendations on how these fluids should be properly stored.”
While it wasn’t a technology solution, Johnson says rather than just say “well, it's not ours to deal with”, when the team looked into it, we responded to what the data showed us. She adds that “data is one of the most persuasive things we can have to make change.”
“I think the thing that we do a little bit differently to other sort of implementation teams is that we don't start with the technology and think wow, this is really cool technology, how can we use it? We start with the issue and figure out the best way to address it. That's one of the reasons we've had success because we're bringing a tailored solution to issues our clinicians encounter rather than trying to shove a square peg in a round hole in saying we’ve just purchased this technology, now what are we going to do with that?”
The team is currently working on a new technology solution to reduce transfers from regular medical wards to the ICU. Smart Beds, which can continuously monitor vital signs, provide alerts to nurses and create opportunity for timely intervention. The pilot project will activate monitoring on a select number of beds to decrease transfers to the ICU.
Self-administered IV antibiotics
Johnson’s team is also involved in a study in Eastern and Western zones to see if the self-administering of IV antibiotics could reduce pressure on the Continuing Care system.
Sometimes the only thing that keeps people in hospital is that they need a nurse to give them IV antibiotics. Although antibiotics can be given at home by community care nurses, if there isn’t capacity to provide the service, patients end up with lengthier stays.
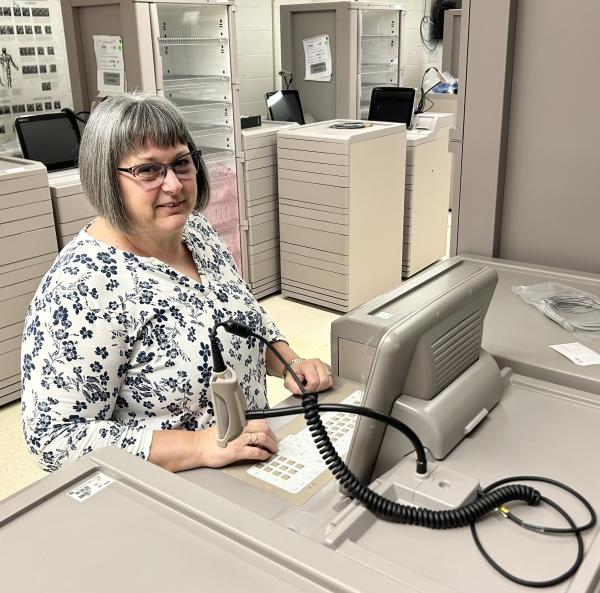
The team did some cross-Canada research and found areas where patients are taught to give themselves IV antibiotics. A new IV pump is now available in Canada which is specifically designed for patient use. Sue says it’s an innovative solution that could potentially relieve pressure on our system.
Dr. Johnson is an internationally educated Registered Nurse from the UK with a PhD in law and sociology with a focus on healthcare law and ethics. She says she always wanted to be a nurse but had no idea what path nursing would take her, or the opportunities that would present themselves. It took her to a variety of bedside specialties, to research, and teaching. Until 2019, Sue says the kind of role she has now didn’t even exist.
“That's what's so wonderful about my profession, there are so many places it can go.”



